Despite the prevalence of low back pain – estimated to affect 1 in 3 adults over the age of 50 – getting an accurate diagnosis and effective treatment to fix the problem is surprisingly difficult. Here, I discuss one very common cause of low back pain which is easily fixed, but frequently missed – dysfunction of the sacroiliac joints.
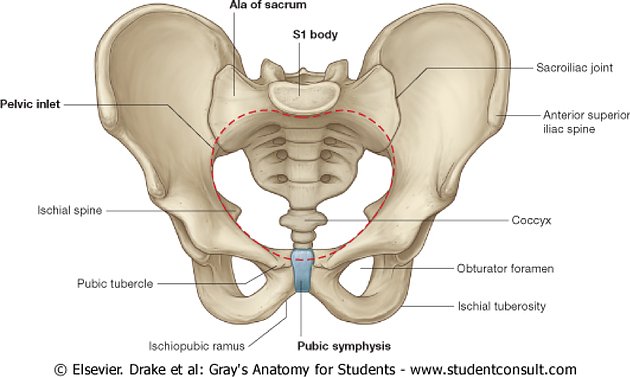
The bony ring of the pelvis is made up of three bones – two innominate or “hip” bones joined at the front by a flexible joint called the pubic symphysis, and the wedge-shaped sacrum at the base of the lumbar spine. The joints between the innominate bones and the sacrum are the sacroiliac (SI) joints.

The pubic symphysis (front) and two sacroiliac joints (rear).
The pelvic joints are supported by strong ligaments, and are therefore less mobile than the spine itself, but nevertheless they are designed to allow a small amount of movement, providing a “shock-absorber” function for the rest of the body. Problems commonly occur when the mobility of one SI joint becomes restricted.
This can build up slowly – for example, as a result of muscular tightness in any of the muscles crossing the joint (commonly the gluteal, piriformis or psoas muscles) or can have a sudden onset – perhaps the jarring from a fall or unexpected slip or step, which causes the connective tissue to tighten.
Symptoms range from a dull ache felt on one side of the low back near the spine or into the upper buttock, to pain radiating round into the groin or down the back of the leg. Acute SI problems can give much sharper pain, worse for weight-bearing and often described as the leg “giving way”. Sitting down and getting up out of low chairs will often cause problems, as will turning over in bed.

The sacroiliac joints are surrounded by strong ligaments and crossed by muscles such as the piriformis, shown here.
Sacroiliac dysfunction is estimated to account for up to 30% of all low back pain, but remains hugely under-diagnosed in the UK. Several factors contribute to this. Firstly, the symptoms are very similar to other common causes of back pain, such as degenerative disc disease or spinal arthritis. Secondly, medical imaging modalities such as X-ray or MRI scans are unable to identify SI dysfunction, as this is a joint movement disorder, without any visible structural change. Therefore, all too often, asymptomatic age-related arthritic changes seen on lumbar spine X-rays are being misdiagnosed as the cause of the pain. For this reason, NICE guidelines now discourage routine imaging for low back pain.
Accurate diagnosis of SI joint dysfunction involves assessing posture, gait and the active range of movement available in the hips, pelvis and low back. This should be followed by a careful examination of each of the pelvic and lumbar joints individually, using a combination of springing, articulation and special orthopedic tests. The tone of each of the muscles crossing the SI joints, and neighbouring muscles acting on the pelvis as a whole, is then assessed. Testing should always be performed by a specialist in musculoskeletal disorders, such as an osteopath, chiropractor or physiotherapist.
The good news is that sacroiliac dysfunction is completely treatable. If it has been caused by a gradual build-up of underlying muscular imbalance, and your symptoms are mild, you can simply stretch the tight muscles (and strengthen the weak ones) daily, to remove the shearing forces across the pelvis, and the natural movement of each SI will slowly return. Some gentle yoga is excellent for maintaining a healthy balanced pelvis.
If your symptoms are more persistent and are not responding to physical activity, or if the joint has been locked by a trip or fall, you should consider consulting a musculoskeletal specialist to get the problem properly assessed and treated. Osteopaths can treat SI dysfunction very effectively, using a combination of stretching, rhythmic joint mobilisations and manipulations, and gentle soft tissue techniques to treat restriction, balance muscles and restore proper movement through the body. They will also advise you on self-care to keep the pelvis moving properly in the future, so you can get back to doing what you love.
About the author:
Marianne Carpenter is a lecturer at Swansea Medical School and a consultant osteopath at Bath Spa Osteopathy, near Green Park Station.