April is IBS awareness month, so here is our helpful guide to the symptoms and treatments available for this common condition.
WHAT IS IRRITABLE BOWEL SYNDROME (IBS)?
The World Gastroenterology Organisation describes IBS as a chronic functional bowel disorder, characterised by intermittent abdominal pain or discomfort, which is usually associated with bloating and a change in bowel habit.
IBS is a common complaint, estimated to affect around 1 in 10 people in the UK. It generally affects those aged between 15-65 with a peak in prevalence in the third and fourth decade. Women are more likely to be affected than men.
This disorder can be classified into several sub-types depending on the predominant bowel symptoms. IBS-C is characterized by constipation and is more common in women, while IBS-D is a diarrhea-predominant subtype more common in men. Suffers may experience a mixture of both symptoms (IBS-M).
Patients with IBS frequently have other co-existing conditions such as fibromyalgia, chronic pelvic pain or chronic fatigue syndrome.
The causes are poorly understood, but research suggests that IBS is linked to changes in gut bacteria populations. The condition can be triggered by gut infections, antibiotic use, major life events causing severe stress, and abdominal or pelvic surgery. Certain foods appear to trigger episodes in some individuals. Whilst the symptoms can have a severe impact on quality of life, IBS is not associated with any increased risk of bowel cancer or Inflammatory Bowel Disease (IBD).
WHAT TREATMENTS ARE AVAILABLE FOR IBS?
As the causes of IBS are poorly understood, it is unsurprising that there is little consensus on the best treatment approaches.
Medications for IBS
The National Institute for Health and Care Excellence (NICE) guidelines recommend a number of medications for the suppression of IBS symptoms. These include anti-spasmodic drugs to relieve pain, and anti-diarrheal or laxative medication depending on the predominant bowel symptoms. Tricyclic antidepressants (TCAs) and selective serotonin re-uptake inhibitors (SSRIs) are sometimes used, although these are associated with a significant risk of adverse effects in around 1 in 3 patients.
Probiotics for IBS
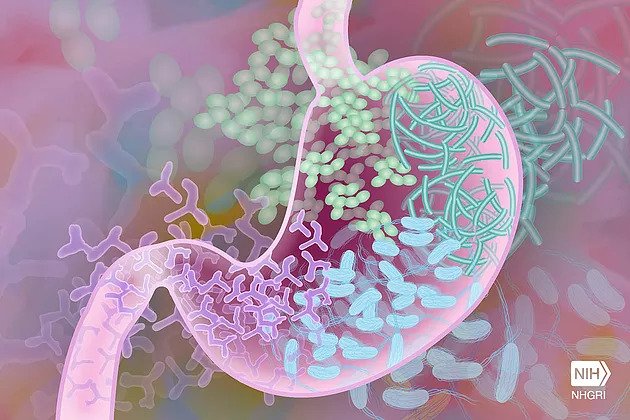
The healthy human gut is home to over 500 bacterial species, weighing around 1kg in total. These “good” bacteria- called commensals- play a vital role in our health, from digestion and the provision of various nutrients (for example, production of Vitamin K) to their role in immunity and even emotional wellbeing. These commensal bacteria usually exist in harmony with our bodies, but the healthy mix of species can be adversely affected by invading bacterial infections, high levels of stress, antibiotic medications and particular foods and drinks, allowing less beneficial bacteria to flourish.
Probiotics are “good bacteria” that can be introduced to the gut– usually in pill or capsule form – to alter the balance back towards a healthy population of commensals. The best evidence for probiotic use in IBS relates to a particular strain called Bifidobacterium Infantis.
Diet for IBS
Due to the impact that various food groups can make on commensal populations, diet is likely to play a key role in managing IBS symptoms. Certain foods are known triggers and should be avoided; these include fatty, fried or processed foods, caffeine, alcohol, and milk products. Adopting a FODMAP diet, and adding oats and linseed to the diet may help relieve some symptoms.
Advice should be sought from a qualified dietician or recommended nutritionist who specialises in IBS diets. Many therapists offer nutritional advice, but the quality of that advice can vary – dieticians are the only nutrition experts regulated by UK law. You can click here for an IBS Food Fact Sheet from the British Dietetic Association.
Peppermint Oil for IBS
Peppermint has traditionally been used for the relief of digestive pain. Studies have suggested peppermint oil is superior to placebo in relieving the symptoms of IBS.
Hypnotherapy and CBT for IBS
Hypnotherapy or Cognitive Behavioral Therapy (CBT) are both recommended by NICE and may be an effective way to relieve the stress and anxiety contributing to IBS symptoms. Altering lifestyle to reduce or avoid stress, and the use of meditation or relaxation techniques may also help.
Osteopathic Treatment for IBS
Osteopathy is accepted as an effective treatment for functional digestive problems. A number of small studies have provided some preliminary evidence for the positive effects of osteopathic treatment on IBS symptoms. For example, in a randomised, controlled trial (RCT) of 39 patients, published in the Journal of Gastroenterology and Hepatology, patients treated with osteopathy reported a 68% improvement in their symptoms. However, further research is needed to establish a reliable evidence base for osteopathy as an effective treatment for IBS.
About the Author
Marianne Carpenter is a registered osteopath and clinical anatomist. She teaches at Swansea Medical School and works in private practice at Applewood Osteopathy in Bath.